When comparing the efficacy of hydrochlorothiazide and chlorthalidone in managing hypertension, hydrochlorothiazide demonstrates comparable effectiveness in lowering both systolic and diastolic blood 1 pressure.
Although chlorthalidone is often noted for its longer duration of action and potentially greater blood pressure reduction, hydrochlorothiazide remains effective for many patients, achieving significant blood pressure 1 control with a lower incidence of side effects.
This makes hydrochlorothiazide a reliable option for managing hypertension, particularly for patients who benefit from its favourable 1 safety profile without compromising efficacy.
In conclusion, according to the DCP study, hydrochlorothiazide has a comparable efficacy as chlorthalidone and it effectively controls blood pressure with a favorable safety profile, making it a1,2 reliable choice for managing hypertension.
When choosing between hydrochlorothiazide and chlorthalidone for patients with high cardiovascular (CV) risk, hydrochlorothiazide may be the more suitable option, particularly for those without a prior history of 1,2 myocardial infarction (MI) or stroke.
Studies, including findings by Ishani et al., suggest that hydrochlorothiazide is associated with fewer adverse effects and 2 remains effective in managing blood pressure.
Hydrochlorothiazide's safety profile makes it a better choice for patients at 2 high CV risk without prior MI or stroke.
Hydrochlorothiazide is generally preferred for patients with high cardiovascular risk, especially in those without a history of MI or stroke, due to its 1,2 favorable efficacy and safety profile.
In patients at high risk of electrolyte imbalances, hydrochlorothiazide is often preferred over chlorthalidone due to its shorter duration of action, 1 which tends to cause less severe potassium depletion.
This makes hydrochlorothiazide a safer option for those vulnerable to 1 hypokalaemia.
Additionally, combining hydrochlorothiazide with potassium-sparing diuretics can help manage hypertension effectively while reducing the risk 1 of electrolyte disturbances.
As compared to Chlorthalidone, hydrochlorothiazide is associated with 30% reduced risk of hyponatraemia and 2.7 times reduced risk of 2 hypokalaemia.
Hydrochlorothiazide is preferred for patients at high risk of electrolyte imbalances due to its shorter duration of action and reduced risk of 1,2 hypokalaemia.
Yes, diet plays a vital role in managing electrolyte imbalances for patients on thiazide diuretics. To counteract thiazide-induced hypokalaemia, patients should incorporate potassium-rich foods like bananas, oranges, and spinach into their diet. It's equally important to manage sodium intake; maintaining a moderate sodium level is crucial, as excessive sodium can worsen fluid retention, while too little sodium may increase the risk of hyponatremia.
Proper hydration is necessary, but excessive fluid intake should be avoided to prevent electrolyte dilution. Including foods rich in magnesium and calcium also supports overall health and helps maintain electrolyte balance. Regular monitoring of electrolyte levels is essential to guide dietary adjustments, ensuring effective management of hypertension while minimizing risks.
Diet is essential in managing electrolyte imbalances for patients on thiazide diuretics, with an emphasis on potassium-rich foods and carefully managed sodium intake to prevent hyponatremia.
If patients on thiazide diuretics experience low sodium (hyponatremia) or potassium (hypokalaemia) levels, the recommended course of action involves several key steps:
Adjusting the dose, supplementing electrolytes, and making dietary changes are key steps before considering discontinuation of thiazide diuretics.1,2
Globally, hydrochlorothiazide is the most widely used thiazide diuretic due to its extensive clinical use, affordability, and broad acceptance in hypertension management. It has been available for more than 50 years and is most commonly prescribed antihypertensive drug worldwide with its presence in more than 130 million prescriptions. It has been established that monotherapy with hydrochlorothiazide has been shown to reduce CV morbidity or mortality.
Hydrochlorothiazide is recommended by multiple guidelines and has demonstrated significant benefits in reducing blood pressure and cardiovascular risk. Despite some debate and emerging alternatives, hydrochlorothiazide's long track record, safety profile, and effectiveness make it a reliable choice for many patients. As per a study by Emerson L, 2023, 25 mg of hydrochlorothiazide is used in 95% of the population.1,2
Hydrochlorothiazide has more global acceptance and usage due to its long track record, affordability, and effectiveness in managing hypertension and a part of 95% thiazide diuretic combinations.1,2
Yes, there are notable differences in the efficacy and side effect profiles of thiazide diuretics between white and black individuals. According to a study comparing hydrochlorothiazide and chlorthalidone, both medications effectively reduce blood pressure but with some racial differences. In white patients, chlorthalidone demonstrated a greater reduction in both systolic and diastolic blood pressure compared to hydrochlorothiazide. However, more significant blood pressure reduction came with an increased risk of adverse metabolic effects, such as hypokalemia and hyperuricemia.
In black patients, chlorthalidone also provided a slightly better reduction in blood pressure than hydrochlorothiazide, but the difference was less pronounced compared to white patients. Importantly, black patients treated with chlorthalidone experienced higher rates of adverse effects, such as hypokalemia, compared to those treated with hydrochlorothiazide. Additionally, black patients on chlorthalidone were more likely to require potassium supplementation.
Chlorthalidone may offer superior blood pressure reduction compared to hydrochlorothiazide in both white and black patients, but it is associated with a higher risk of adverse metabolic effects, especially in black individuals. This suggests that the preference for chlorthalidone over hydrochlorothiazide may need reconsideration, particularly in black patients, due to the differences in efficacy and side effect profiles.
As per American Heart Association, International Society of Hypertension, Indian Society of Hypertension & European Society of Hypertension, Angiotensin receptor blockers (ARBs)+ diuretics are recommended as a first line treatment for hypertension, especially for patients with:1-4
Guidelines recommend thiazide diuretics as a first-line treatment for hypertension, with emphasis on their efficacy in managing blood pressure.1-4
Thiazide diuretics are often the first choice for hypertensive patients in specific groups as follows:
Thiazide diuretics are often the first choice for hypertensive patients, particularly those who are black, elderly, having cardiovascular risk, or have mild to moderate hypertension.1-3
The ideal dose of thiazide diuretics, as recommended by ACC/AHA, is crucial for achieving effective blood pressure control while minimizing side effects.
The minimum effective dose for all thiazide diuretics is 12.5 mg daily, with an optimal range of 12.5 to 25 mg.
Lower doses, such as 6.25 mg, are considered sub-optimal for effective management of hypertension and may not provide sufficient benefit.
Therefore, 12.5 mg is generally preferred as the starting dose due to its balanced efficacy and safety profile.1-2
The ideal starting dose for thiazide diuretics, including hydrochlorothiazide, is 12.5 mg daily, as recommended by ACC/AHA. This dose ensures optimal efficacy while minimizing the risk of adverse effects, making it the preferred choice over sub-optimal doses or higher doses of chlorthalidone.1-2
In older adults with varying levels of kidney function, hydrochlorothiazide is generally preferred over chlorthalidone. A recent cohort study found that chlorthalidone was associated with a higher risk of a 30% or more decline in estimated glomerular filtration rate (eGFR), as well as a greater incidence of cardiovascular events and hypokalemia compared to hydrochlorothiazide. The risk of hypokalemia was somewhat reduced in patients with lower kidney function.
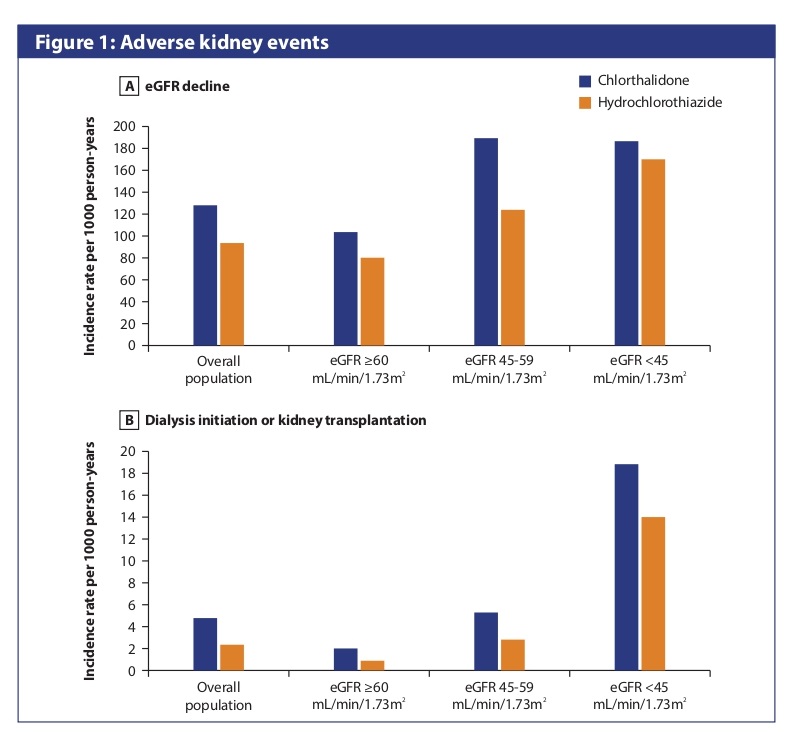
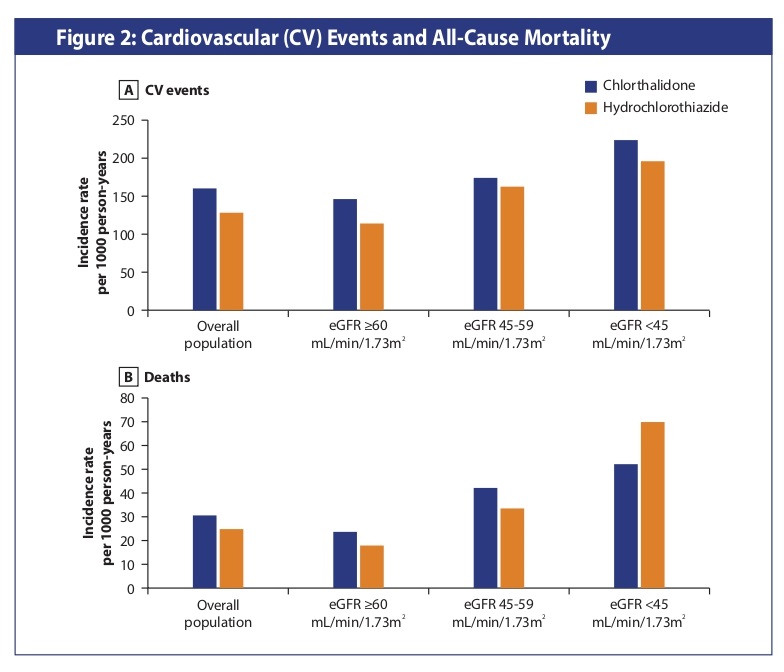
For patients with chronic kidney disease (CKD), hydrochlorothiazide is often preferred over chlorthalidone because it poses a lower risk of worsening kidney function and has a better safety profile for potassium levels and cardiovascular benefits.
Chlorthalidone is associated with a higher incidence of hyperuricemia compared to hydrochlorothiazide.
Therefore, hydrochlorothiazide may be preferred for patients with a history of gout or hyperuricemia. In a study that compared the incidence of new-onset gout with diuretic therapy, the incidence of gout for the chlorthalidone group was higher than the hydrochlorothiazide group.1,2
Hydrochlorothiazide is preferred for patients with a history of gout or hyperuricemia due to its lower incidence of hyperuricemia compared to chlorthalidone. 1,2
For diabetic patients with hypertension, hydrochlorothiazide is often preferred due to its lower impact on glucose metabolism compared to chlorthalidone, which can exacerbate insulin resistance.
Low doses of hydrochlororthiazide are generally preferred to mitigate adverse effects while still providing therapeutic benefits.
Hydrochlorothiazide is often the better option for diabetic hypertensive patients due to its lower impact on glucose metabolism compared to chlorthalidone.
According to IMS Rx data, an average of 67,000 HCPs have prescribed hydrochlorothiazide whereas chlorthalidone has been prescribed by 35,000 doctors, indicating that hydrochlorothiazide is more commonly used compared to chlorthalidone.
In India, Hydrochlorothiazide has almost double the average users than Chlorthalidone.
hypertension, recent analysis highlights significant differences in effectiveness:
As per Cochrane review wherein 90,000 participants were included, thiazide diuretics reduce total cardiovascular events (14.3% versus 13.3%; RR 0.93, 95% CI 0.89 to 0.98) and heart failure (4.4% versus 3.2%; RR 0.74, 95% CI 0.66 to 0.82), with reduced risk of withdrawals due to adverse effects (7.6% versus 6.2%; RR 0.81, 95% CI 0.75 to 0.88), as compared to CCBs.
When used as first-line agents for the treatment of hypertension, thiazide diuretics decreases morbidity outcomes such as cardiovascular events and withdrawals due to adverse effects when compared to CCBs.
© 2024 Reassurance. All Rights Reserved by Reassurance